Reflective Practice in Nursing: Key Models & Benefits
Introduction to Reflective Practice in Nursing
Reflective practice has become an essential component of nursing education and professional development in the UK. It encourages nurses to critically analyze their experiences, fostering continuous improvement and better patient care. By engaging in reflective practice, nurses can deepen their understanding of their professional roles, enhance their decision-making skills, and improve their clinical outcomes.
In this blog post, we will explore the significance of reflective practice in nursing, examine key models used in the field, discuss steps for effective implementation, and highlight the benefits and challenges associated with this practice.
The Importance of Reflection in Nursing
Reflection is a vital skill for nurses. It allows them to pause, think critically about their actions, and understand the implications of their choices. By reflecting on their experiences, nurses can:
- Enhance Clinical Skills: Reflection helps identify areas for improvement and reinforces effective practices.
- Improve Patient Care: By understanding their experiences, nurses can develop better communication and interpersonal skills, leading to improved patient outcomes.
- Foster Professional Development: Reflective practice encourages lifelong learning, helping nurses adapt to new challenges and developments in healthcare.
According to the Nursing and Midwifery Council (NMC), reflection is a crucial aspect of continuing professional development, emphasizing the need for nurses to regularly engage in reflective practice to maintain high standards of care.
Key Reflective Models Used in Nursing
Several reflective models are utilized in nursing practice, with each offering unique approaches and insights. The most commonly used models include:
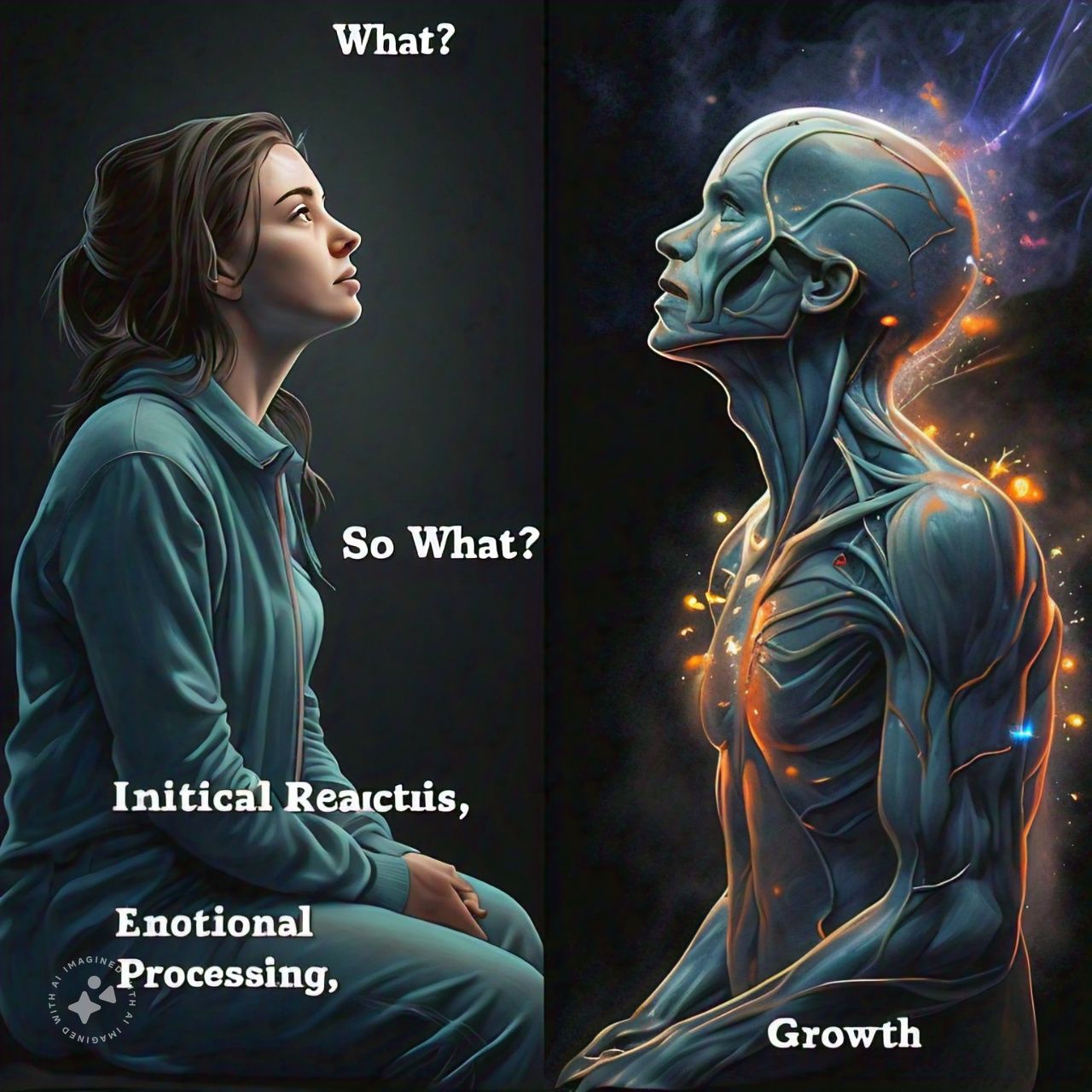
Rolfe’s Reflective Model
Rolfe’s Reflective Model is based on three fundamental questions: “What?”, “So What?”, and “Now What?”. This model is particularly useful for students and practitioners seeking a structured approach to reflection.
- What?: This question prompts the nurse to describe the situation, including key events, actions taken, and the roles of others involved.
- So What?: This encourages analysis of the situation’s significance, exploring feelings, thoughts, and lessons learned.
- Now What?: Finally, this question focuses on future actions and improvements based on the reflection.
Using Rolfe’s model helps nurses systematically analyze their experiences, leading to enhanced understanding and professional growth.
Gibbs’ Reflective Cycle
Another widely adopted model is Gibbs’ Reflective Cycle, which consists of six stages: description, feelings, evaluation, analysis, conclusion, and action plan. This model encourages deeper exploration of the experience and its impact.
- Description: Describe the experience without judgment.
- Feelings: Reflect on emotional responses to the event.
- Evaluation: Assess what went well and what didn’t.
- Analysis: Delve into the reasons behind the outcomes.
- Conclusion: Identify lessons learned.
- Action Plan: Develop strategies for improvement.
Gibbs’ cycle provides a comprehensive framework for reflection, enabling nurses to explore their experiences thoroughly and draw meaningful conclusions.
Steps to Implement Reflective Practice
To effectively implement reflective practice in nursing, consider the following steps:
- Set Aside Time for Reflection: Allocate specific times for reflection, whether after a shift or during dedicated training sessions.
- Choose a Reflective Model: Select a model that resonates with you, such as Rolfe’s or Gibbs’, to guide your reflection.
- Engage in Critical Thinking: Analyze your experiences critically, considering different perspectives and outcomes.
- Document Your Reflections: Write down your reflections in a journal or electronic format to track your growth and development.
- Seek Feedback: Share your reflections with peers or mentors to gain additional insights and perspectives.
- Create an Action Plan: Based on your reflections, develop a plan for improving your practice and addressing any identified areas for growth.
Tips for Effective Reflection
- Be Honest: Allow yourself to be vulnerable and acknowledge areas for improvement.
- Be Specific: Focus on particular events or experiences to make your reflections meaningful.
- Use Prompts: Utilize prompts to guide your thinking and help you delve deeper into your experiences.
- Stay Open-Minded: Approach reflection with a willingness to learn and grow from your experiences.
Benefits of Reflective Practice for Nurses
Engaging in reflective practice offers numerous benefits for nurses, including:
- Enhanced Self-Awareness: Reflective practice fosters greater self-awareness, helping nurses recognize their strengths and weaknesses.
- Improved Critical Thinking: Regular reflection sharpens critical thinking skills, enabling nurses to make more informed decisions.
- Greater Accountability: Reflection encourages accountability for one’s actions and decisions, promoting ethical practice.
- Increased Confidence: As nurses gain insights from their reflections, they become more confident in their abilities and decision-making.
- Better Team Collaboration: Reflective practice can enhance communication and collaboration within healthcare teams, leading to improved patient care.
Challenges in Reflective Practice
While reflective practice is beneficial, several challenges may arise, including:
- Time Constraints: In busy healthcare environments, finding time for reflection can be difficult.
- Emotional Barriers: Reflecting on challenging experiences can evoke strong emotions, making it hard to engage in reflection.
- Lack of Support: Some nurses may lack support from colleagues or management, hindering their ability to reflect effectively.
Overcoming Challenges
To overcome these challenges, consider the following strategies:
- Integrate Reflection into Routine: Make reflection a part of your daily practice, incorporating it into your workflow.
- Create a Supportive Environment: Foster a culture of reflection within your team, encouraging open discussions about experiences and lessons learned.
- Utilize Technology: Use digital tools or apps to facilitate reflection and documentation, making the process more efficient.
Conclusion
Reflective practice is an essential component of nursing that promotes continuous learning, improved patient care, and professional development. By engaging with reflective models like Rolfe’s and Gibbs’, nurses can systematically analyze their experiences, leading to enhanced self-awareness and better clinical outcomes.
As the healthcare landscape continues to evolve, the ability to reflect critically on one’s practice will remain crucial. By overcoming challenges and embracing reflection as a regular practice, nurses can not only enhance their skills but also contribute to the overall quality of care in the UK healthcare system.
Additional Resources
For further reading and resources on reflective practice in nursing, consider exploring the following:
- The Importance of Reflection in Nursing Practice – Nursing and Midwifery Council
- Gibbs’ Reflective Cycle Explained – Coursera





